
Symptomatic treatment is possible with antidepressants and sodium oxybate.
#Atypical cataplexy series
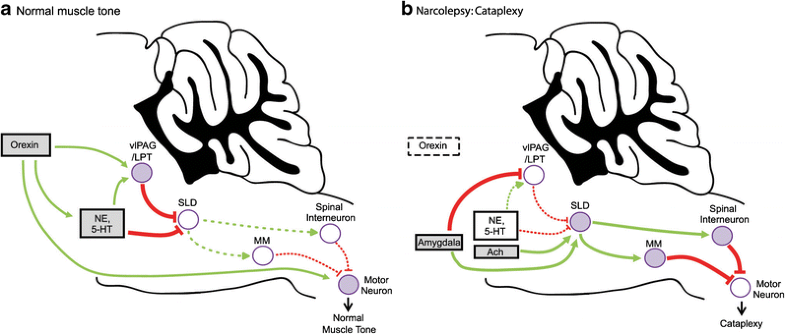
Over time, these severe symptoms evolve to the milder adult phenotype, and this pattern is crucial to recognize when assessing the outcome of uncontrolled case series with potential treatments such as immunomodulation. In some patients, atypical cataplexy turns out to be real cataplexy, while in others, it refers to non-cataplectic events. HLA DQB106 02 typing is useful when it is negative in the case of atypical cataplexy as this reduces the probability of NT1. Cataplexy is sudden, uncontrollable muscle weakness or paralysis that occurs. Cataplexy shows remarkable differences in childhood compared to adults, with profound facial hypotonia and complex active motor phenomena. To complicate matters, a distinction between typical and atypical cataplexy has been made in the literature, although atypical cataplexy has not been clearly defined and codified. VRAYLAR is an atypical antipsychotic indicated for the: Treatment of. Currently, the diagnosis of cataplexy is made almost solely on clinical grounds, based on history taking and (home) videos. Childhood narcolepsy, with its profound facial hypotonia, can be confused with neuromuscular disorders, and the active motor phenomenona resemble those found in childhood movement disorders such as Sydenham's chorea. They can be differentiated from cataplexy using thorough history taking, supplemented with (home)video recordings whenever possible. Cataplexy mimics include syncope, epilepsy, hyperekplexia, drop attacks and pseudocataplexy. 1.4), that atypical cataplexy has no diagnostic value, thus the need to call cataplexy only with typical presentations. Next to narcolepsy, cataplexy can sometimes be caused by other diseases, such as Niemann-Pick type C, Prader Willi Syndrome, or lesions in the hypothalamic or pontomedullary region. Moreover, childhood cataplexy differs from the presentation in adults, with a prominent facial involvement, already evident without clear emotional triggers ('cataplectic facies') and 'active' motor phenomena especially of the tongue and perioral muscles. The expression of cataplexy varies widely, from partial episodes affecting only the neck muscles to generalized attacks leading to falls. Although cataplexy is rare, its recognition is important as in most cases, it leads to a diagnosis of narcolepsy, a disorder that still takes a median of 9 years to be diagnosed. This review describes the diagnosis and management of cataplexy: attacks of bilateral loss of muscle tone, triggered by emotions and with preserved consciousness.


 0 kommentar(er)
0 kommentar(er)
